
Copyright 2009-2014 Saviz Inc. All rights reserved.
Hemorrhoid:
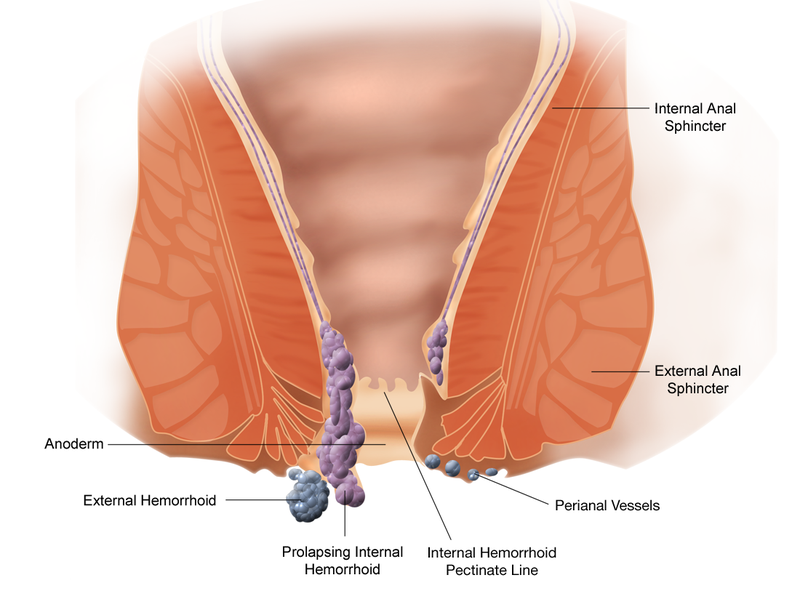
Hemorrhoids are divided into two types, external and internal. External hemorrhoids are located in the distal one-third of the
anal canal, distal to the dentate line, and are covered by anoderm Internal hemorrhoids are located proximal to the dentate line and are covered by columnar or transitional epithelium. Because this overlying tissue is viscerally innervated, it is not sensitive to touch, pain, or temperature, making it easily amenable to office procedures. Internal hemorrhoids are further subclassified into degrees based on size and clinical symptoms .
Mixed or combined hemorrhoids are defined as the internal and external hemorrhoids
Symptoms:
Patients with anal complaints from whatever etiology frequently present at the office complaining of ōhemorrhoids or piles.ö Many patients referred or coming into the office complaining of ōhemorrhoidsö frequently are found to have other anal problems such as pruritus ani, anal fissures, fistulas, and skin tags. A careful history and physical examination including anoscopy by an experienced individual is mandatory and will frequently lead to the correct diagnosis. The presence, quantity, frequency, and timing of bleeding and prolapse should be noted. Patients with hemorrhoid disease may complain of bleeding, mucosal protrusion, pain, mucus, discharge, difficulties with perianal hygiene, a sensation of incomplete evacuation, and cosmetic deformity. A thorough dietary and medication history should also be done because certain medications, diets, and or dietary indiscretions cause or exacerbate constipation or diarrhea. Symptoms from external hemorrhoids are usually secondary to thrombosis and physical examination shows a tender, bluish-colored lump at the anus distal to the dentate line
associated with acute pain. Thrombosed external hemorrhoids can bleed secondary to pressure necrosis and subsequenthe presence of both internal and external hemorrhoids ulceration of the overlying skin. External skin tags are folds of skin that arise from the anal verge. These tags may be the end result of prior episodes of thrombosed external hemorrhoids. Enlarged skin tags or external hemorrhoids may interfere with anal hygiene leading to perianal burning or pruritus. Internal hemorrhoids are painless unless thrombosis, strangulation, gangrene, or prolapse with edema occurs. Despite what is written, patients will frequently come to the office complaining of ōpainful hemorrhoidsö even when none of these conditions exist. Once other sources of pain are ruled out, careful inquiry regarding the description of their pain further elucidates that patients frequently describe their anal pain as ōburningö in nature. This may be secondary to perianal irritation from mucous or fecal leakage leading to secondary pruritus ani. Bleeding from internal hemorrhoids is bright red and associated with bowel movements. The bleeding usually occurs at the end of defecation. The patient may complain of blood dripping or squirting into the toilet or blood on the toilet tissue. Bleeding may also be occult leading to guaiac-positive stools or rarely to anemia. Prolapse of the hemorrhoid cushions may manifest itself as an anal mass, mucous discharge, or a sensation of incomplete evacuation. The examiner should ascertain whether the hemorrhoids reduce spontaneously or require manual reduction.
Treatment:
Treatment for symptomatic internal hemorrhoids varies from simple reassurance to operative hemorrhoidectomy. Treatments are classified into three categories) dietary and lifestyle modification; nonoperative/office procedures; and operative hemorrhoidectomy. In general, less symptomatic hemorrhoids, such as those that cause only minor bleeding, can be treated with simple measures such as dietary modification, change in defecatory habits, or office procedures. More symptomatic hemorrhoids such as third or fourth degree are more likely to require operative intervention.
Dietary and Lifestyle Modification :
Because prolonged attempts at defecation, either secondary to constipation or diarrhea, have been implicated in the development of hemorrhoids, the main goal of this treatment is to minimize straining at stool. This is usually achieved by increasing fluid and fiber in the diet, recommending exercise, and adding supplemental fiber agents (psyllium) to the diet in
patients unable to consume sufficient amounts of fiber in their diets. Despite common teaching, little good evidence exists regarding the benefit of fiber in preventing or managing hemorrhoid disease. Reduced hemorrhoidal bleeding has been shown with the use of psyllium in a double-blind, placebo controlled trial; however, other studies are less favorable.23¢26
Psyllium works in conjunction with water to add moisture to the stool and subsequently decrease constipation. Psyllium may also be therapeutic in treating diarrhea. It may add bulk to liquid stools therefore increasing the consistency and decreasing the volume. Dietary modification with fiber supplementation (psyllium, methylcellulose, calcium polycarbophil) is one of the mainstays of therapy for patients with hemorrhoidal disease. In the majority of cases, symptoms of bleeding and pain improve over a 6-week period. A diet high in fiber (20¢35 g/day) including the consumption of plenty of fruits and vegetables is recommended especially if the patient has a history of constipation or straining. A common problem with fiber supplementation is noncompliance because of either poor palatability or symptoms of bloating, increased flatus, and abdominal cramps. Compliance is improved by starting at lower doses and slowly increasing the quantity of fiber ingested until the desired stool consistency is achieved.
If dietary modification fails to relieve symptoms, then further therapy is indicated. Frequently, a change in defecatory habits will resolve symptoms. Oftentimes, simply asking an individual to curtail reading on the commode resolves the hemorrhoidal symptoms.
Lifestyle and dietary modifications along with ruling out proximal sources of bleeding are all that is required for the majority of patients complaining of hemorrhoidal disease.
Office Treatments :
Rubber Band Ligation
Rubber band ligation is a method of tissue fixation and one of the most widely used techniques in the United States. It can be used to treat first-, second-, and third-degree internal hemorrhoids. The most common method currently in use for the outpatient treatment for hemorrhoids was originally described The rubber band is placed on the redundant mucosa a minimum of 2 cm above the dentate line which causes strangulation of the blood supply to the banded tissue, which sloughs off in 5¢7 days leaving a small ulcer that heals and fixes the tissue to the underlying sphincter. Rubber band ligation is frequently recommended for individuals with first- or second-degree hemorrhoids and, in some circumstances, third-degree hemorrhoids.
Several commercially available types of hemorrhoid ligators are available including a suction ligator. simplify the banding procedure for both patient and surgeon This single-operator ligator, with its own suction mechanism, was designed for use without the need of an assistant or an anoscope. By pointing the ligator directly toward the appropriate site and by measuring the distance from the anal margin using reference markings on the ligator, the bands can be placed accurately in a blind manner inside the rectum for the treatment of symptomatic internal hemorrhoids.
OÆRegan reported a 97% success rate with two major complications (one episode of bleeding and one of perianal sepsis) in 480 patients.
Rubber band ligation can be performed safely with the patient in various positions; however, the prone jackknife position provides the best exposure. Anesthesia is not required for this procedure. Rectal preparation with enemas is not required but may be used if desired.
Infrared Photocoagulation, Bipolar Diathermy,
and Direct-Current Electrotherapy are other modalities of office used techniques for therapy of hemorrhoids
External Hemorrhoids:
Acute Thrombosis
Patients with a thrombosed external hemorrhoid typically present with complaints of a painful mass in the perianal region. The pain is frequently described as burning in nature. The pain associated with the abrupt onset of an anal mass usually peaks at around 48 hours and subsides significantly after the fourth day.The skin overlying the thrombosed hemorrhoid may necrose and ulcerate, resulting in bleeding, discharge, or infection.
Operative Hemorrhoidectomy :
Hemorrhoidectomy is indicated for patients with symptomatic
combined internal and external hemorrhoids who have
failed or are not candidates for nonoperative treatments. This
would include patients with extensive disease, patients with
concomitant conditions such as fissure or fistula, and patients
with a preference for operative therapy. Only about 5%¢10% of
patients need surgical hemorrhoidectomy. Recurrence with
operative hemorrhoidectomy is uncommon and hemorrhoidectomy
is the most effective treatment for hemorrhoids, especially
those that are third degree. Hemorrhoidectomy can be
performed using a variety of techniques or instruments; however,
most are variants of either a closed or open technique.
The Milligan-Morgan technique (open) is widely used in the
United Kingdom. It involves excision of the
external and internal hemorrhoid components leaving the skin
defects open to heal by secondary intention over a 4- to 8-week
period. The Ferguson hemorrhoidectomy (closed) involves
excision of the external and internal hemorrhoid components
with closure of the skin defects primarily
Stapling Technique:
The stapling procedure can be done with the patient in the
prone jackknife, lithotomy, or left lateral position while under
local, spinal, or general anesthesia. A circular anal dilator is
introduced into the anal canal, which reduces the prolapsed tissues.
The obturator is removed, and the prolapsed tissue falls
into the lumen of the dilator. A circumferential pursestring
suture is placed 4¢6 cm above the dentate line into the submucosa.
The circular stapler is opened and the head is introduced
proximal to the pursestring. The pursestring sutured is tied and
the suture threader is used to pull the free ends of the pursestring
suture through a pair of holes on the lateral sides of the
stapler. Traction is applied to the pursestring while the stapler
is being closed, which causes the prolapsed mucosa and some
hemorrhoidal tissue to be drawn into the casing. The stapler is
fully tightened and then fired. The instrument should be left
closed for 20 seconds after firing to enhance hemostasis. The
staple line should be carefully examined for hemostasis and
any bleeding areas should be oversewn. Anoscopic examination
will reveal persistent internal hemorrhoids. It is important
to remember that this technique does not completely excise the
hemorrhoids; rather, it returns the tissues to their physiologic
location. The circular specimen will contain the excised tissue
and the pursestring suture.
Posthemorrhoidectomy Hemorrhage:
Severe hemorrhage after hemorrhoidectomy is a rare complication
occurring in approximately 2%. Traditionally, sepsis of the ligated pedicle has
been considered an important etiological factor, although this
has been challenged by a recent study by Chen et al. who
found male patients and operating surgeon as risk factors. The
majority of patients will respond to packing or tamponade
with a Foley catheter balloon. Approximately 15%¢20% of
patients may need suture ligation to control the postoperative
bleed. Initial rectal irrigation has been suggested as a technique
to separate patients that have stopped bleeding from
those that need to go to the operating room. Another helpful
technique is to irrigate the rectum free of clots and blood
at the initial hemorrhoid operation, to prevent postoperative
passage of old clots that could cause clinical confusion.
About Hemorrhoid

.jpg)





.jpg)